Red and Green bed days
Red and green bed days are value qualifiers of how impactful a day was for healthcare delivery as part of a ‘visual management system’ according to NHS England, and can be used for both acute care, delivered in hospitals, and community care.
Below we expand on the definitions of red days and green days.
What is a Red day?
A red day is a day of no value for a patient. That doesn’t necessarily mean they don’t receive any care, but the wider impact or implications of that healthcare are minimal.
NHS England asks two questions to determine if a day has been a red day:
- Could the care or interventions the patient is receiving today be delivered in a non-acute setting?
- If I saw this patient in out-patients, would their current ‘physiological status’ require emergency admission?
NHSE states that if the answers to the above are 1) yes and 2) no then this is a red bed day.
This does overcomplicate it a little though. Red bed days are when things like assessments or procedures don’t happen, so the day was wasted. They are when the patient’s care plan has no estimated date of discharge so they’re vaguely moving through the care journey rather than being regularly progressed. The big one is that a red bed day can be when a patient is getting care that doesn’t require an acute hospital bed.
Ultimately red bed days are about inefficient, ineffective, or inappropriate care delivery.
What is a Green day?
A green day is a day of value for a patient in a clinical setting. They should not be confused with the punk rock band from California…
A lot of what defines the green days is the opposite of the red days: these days are categorised as days where care delivered value to a patient and moved them closer to recovery and hospital discharge. It is a day where planned activities or treatments occurred, and the patient was appropriately occupying an acute hospital bed for their care.
Why the Red to Green approach?
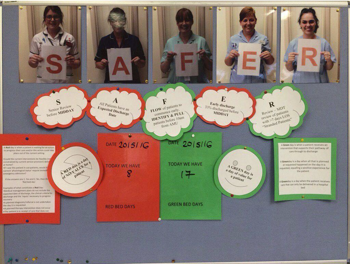
To understand why the Red to Green approach, you must first understand the SAFER rules. The NHS uses the SAFER principle to help guide patient journeys and treatment plans, and it stands for:
- S - Seen (before midday)
- A - Aim (key patient questions + answers)
- F - Flow (right bed, first time + proper preparation)
- E - Early Discharge (assist patient departure)
- R - Recovery (goals + external support services)
The Swansea Bay University Health Board explains that the SAFER principles are used to manage hospital flow, and that the Red to Green approach is an enabler for achieving said care principles.
The goal is a consistent one: to see patients in a prompt fashion, to swiftly establish a care plan including assessment and treatment, and to plot the time this journey will take and an estimated departure time from the acute setting. Depending on the illness or injury and the patient’s overall wellbeing or condition or age, this can vary. Some will need more hospital care, others can quite quickly step away into community support.
The Red to Green approach is important because – as the Swansea health board points out – there’s an initial loss of value in patient delays, but also a double whammy of further costs AND patient deterioration through hospital stays. In their own words: “There is growing recognition that lack of physical activity during hospital stays can have significant negative consequences for patients, especially in older people. Patients lose physical and cognitive abilities within hours if actions aren't taken to prevent deconditioning.”
Red to Green days is an approach that seeks to resolve an existing problem: that patients aren’t at the centre of their own care. They are the user, they are the taxpayer, and they have expectations about service delivery. This obviously manifests more in terms of stress and fear, but it still comes back to that one word: expectation.
With this in mind, the patient flow optimisation that Red to Green days seeks to deliver is about answering questions for the patient by asking them of the clinicians and the healthcare processes. Does the patient know what’s wrong with them? Do they know the plan going forward? What’s the end goal regards assessment or treatment? And the big one – when can they go home?
Lack of clarification is frustrating for the patient, but that stems from communication issues. Some of these are human error, but a lot is the complexity of modern healthcare, which is why providers like The Access Group exist to provide smart solutions to alleviate these new burdens.
How did the Red and Green bed day process come about?
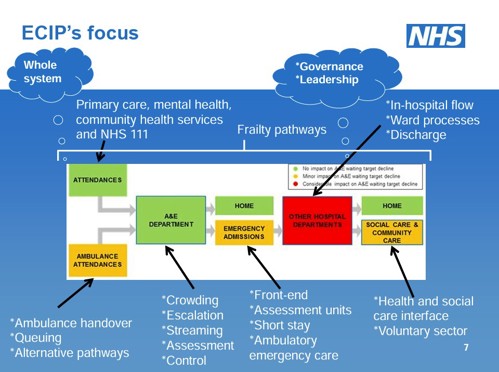
The red and green bed day process is the brainchild of Dr Ian Sturgess; currently the Interim Director of Clinical Transformation at NHS Cornwall and Isles of Scilly ICS but formerly the Clinical Director of the NHS Emergency Care Improvement Programme (ECIP).
Dr Sturgess produced the guide in 2016 and published it over on The Academy of Fabulous Stuff website – a hub for health and care ideas or solutions. A lot of what has been stated by the NHS across different trusts, boards and systems has been lifted or paraphrased from Dr Sturgess’ initial explanation in this guide.
His process was designed to target the aspects of healthcare management that he saw as flawed. The RESPONSE model, which is similar to SAFER, flagged aspects like reviewing, streamlining, planning, and escalation as some of the eight touchpoints along a patient’s journey from admission to discharge and how they could be problematic but also how clinicians should approach these ‘beats’ or milestones of a patient’s journey to keep the patient’s care productive and driving towards the discharge.
What is the Red 2 Green process?
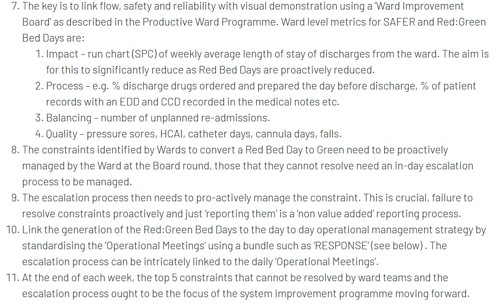
Dr Sturgess laid out the Red 2 Green process in his guide, and has a 11-point schedule for the delivery of this system – as quoted below:
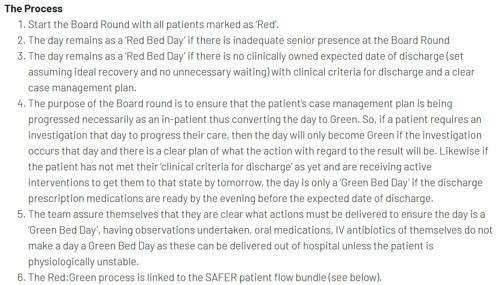
For a more visual explanation of this you can see the below video from the Emergency Care Improvement Programme team and their work with Ipswich Hospital NHS Trust in 2017, where they demonstrate how the SAFER principles are applied to wards and how the Red to Green process is observed.
We should point out that, being several years ago, this process may now be partially or fully digitised, and that this is merely a demonstration of how the system was being implemented in the aftermath of Dr Sturgess’ patient flow improvement scheme.
Case Studies in Health and Social Care
Below we’ve chosen from a large selection of case studies and testimonials sourced across the last few years from within the NHS, to explore the exposure to these red and green days and the sentiment about their implementation and their benefit.
1 - East London NHS Foundation Trust (ELFT)
Our first study is the East London NHS Foundation Trust, taken from a webpage on the red to green approach in Tower Hamlets published by ELFT in 2024.
ELFT has seen a higher demand for healthcare services based on rising population and “increasing complexity and severity of healthcare needs”. This has led the four acute inpatient wards within the Tower Hamlets Centre for Mental Health to take the lead and trial the red and green days.
The trust launched the system in March 2024 during a critical incident, with the goals of reducing average stay durations to 40 days and identifying blockages in the discharge process. Despite difficulties with the manual collection of data for the red 2 green process, feedback from staff was generally positive, though ELFT admitted it needed further investigation before wider deployment would occur to ensure adequate data capture and assessment to deliver appropriate care to patients.
2 - Cheshire and Wirral Partnership NHS Foundation Trust (CWP)
Insights were produced by NHS England in 2018 on Cheshire and Wirral Partnership NHS Foundation Trust (CWP), looking at their project to improve patient flow through mental health inpatient services.
Feedback is fairly minimal unfortunately, but similar to ELFT there were amendments made to improve data recording – though in this case they do talk about utilising an actual Red2Green database. It’s unclear if this is part of their electronic patient record solution or some other software.
The other bit of intel provided is that CWP did report a reduction in time spent on board rounds and more consistency in the Red 2 Green charts as time went by – an indicator of greater clinical understanding and workflow.
3 - Worcestershire Acute Hospitals NHS Trust
This PDF on SAFER and red 2 green comes from May 2016. It lacks intel in terms of conclusions or feedback, but the below image demonstrates how the trust were illustrating their patient flow as part of onboarding staff to the new protocols:
4 – Royal Free London NHS Foundation Trust
The Royal Free in London issued this news statement in 2017 on turning red days green. In it, ward manager Liz Pollard from the Willow Ward spoke about their first month using the Red2Green principles.
“I must admit I was a little hesitant at first, but it truly has been a simple and positive process to implement... Staff tell me they feel it has benefitted both patients and themselves by keeping them focused on what their patients require to provide not just excellent care, but to get them home safely as soon as possible.”
There’s a little more PR spin in the mix too, but the key point is that it did aid the patient journey and discharge processes.
5 – University Hospitals of Leicester NHS Trust
Another from 2017, the University Hospitals of Leicester NHS Trust library has a published paper on their actions regards SAFER and red to green days.
The trust implemented SAFER and red2green as of December 12, 2017, and reported an initial conversion rate of 76%, which translates as… we don’t know. It’s a nice high percentage, but the lack of context is tricky. One would assume it means an improvement in the rate of discharging patients, which is welcome, but assumptions aren’t fact.
What is fact is that University Hospitals of Leicester NHS Trust reported issues with electronic reporting and data quality, with plans to switch to manual data collection in the short term whilst amendments and fixes were implemented. It would be interesting to revisit them and see if improvements had been made for digital assistance and if so, how.
6 – Oxford Academic
Our last study covers an anonymous co-op ward, as explored by Oxford Academic in 2017.
NHS Improvement worked with their Emergency Care Intensive Support Team (ECIST) to utilise the red and green days for increasing efficiency in patient flow. The feedback was an initial drop in team moral, with some clinicians taking personal offence at the recorded causes of red days. The delivery of feedback and other guidance though onboarded said healthcare professionals, and slowly over time there was staff buy-in to the protocols.
The OA findings were that in a two week period, 89 red days were recorded. 53% of those were caused by internal factors that could be overcome, whilst the rest were social services or community related. The response was for the larger NHS trust in the area to develop a red-green app that captures data to find patterns regarding the causes of red days and the patient trends involved.

Patient Satisfaction in Healthcare
One of the two areas not really delved into in this article has been the patient satisfaction element of the red and green bed days. NHS Trusts, health boards, and integrated care boards have talked about the benefit to patients from more efficient and relevant healthcare, but there’s little testimony as to how patients feel about the scheme.
This is unfortunately inevitable, because how do you qualify it or quantify its impact? There are many factors that impact patient flow through a hospital setting, and you can’t isolate the sole impact of the Red and Green days on the patient experience. You can however measure or monitor patient engagement, which is something we’d argue more evidence should be taken on – do patients feel they are being properly engaged through the AIM part of SAFER?
Healthcare & Technology
The other area – that we can and should explore – relates to healthcare technology and how it supports clinical workflow, data capture, and data analysis.
Much of the evidence cited above in our case study section is related to information that came out in the first few years of the NHS trialling and then implementing the red 2 green protocols. This is useful information and insight, but it lacks depth and specificity. We need to know:
- What solutions they were using and are using now.
- What prompts – if any – these solutions are giving.
- What parts of the SAFER process and the red to green days the technology is helping with.
- How reliable is data capture? How accurate is the data captured?
- Are software solutions easy to use? Were they easy to onboard/implement?
- How costly were these solutions and was cost-benefit analysis performed to showcase return on investment?
These are the next step of questions to ask and, given that red to green days are a part of the patient flow process, again we experience the challenge differentiating and isolating the impact of them in specific relation to the red 2 green days. The difference here is that we can use the information gleaned to understand the bigger picture impact of healthcare technology and can extrapolate whether some of these guides – like red to green days – will be quite so necessary in future if software solutions are doing this automatically.
There’s also the argument that without these guides you can’t build the software architecture to support it. It’s not on solutions providers like Access to argue either way, but it’s important that the NHS and industry work in collaboration to identify needs and patterns and push for maximum efficiency.
The Red and Green bed days scheme would not be used to facilitate the SAFER protocols if they weren’t beneficial. The important thing though is to investigate through expert assessment about the pros and cons of the guidance and if anything can be improved.
There were difficulties encountered in the 2016-2018 trial runs, so it’s important that these trialists are spoken to and gauged on their thoughts at the time and their thoughts now: has the system improved, has tech caught up and fixed any issues, or are there problems being swept under the rug because of tight budgets and staff shortages?

 AU & NZ
AU & NZ
 SG
SG
 MY
MY
 US
US
 IE
IE

