How can EHR systems reduce costs?
EHR systems can reduce costs by optimising existing care processes. Efficiency is important in any workplace, but in health and care especially, and it is this return on investment that makes EHR systems really worthwhile.
Our software page on electronic patient records gives the below example of the return on investment that we see at Access when providing EPR solutions for partner organisations.
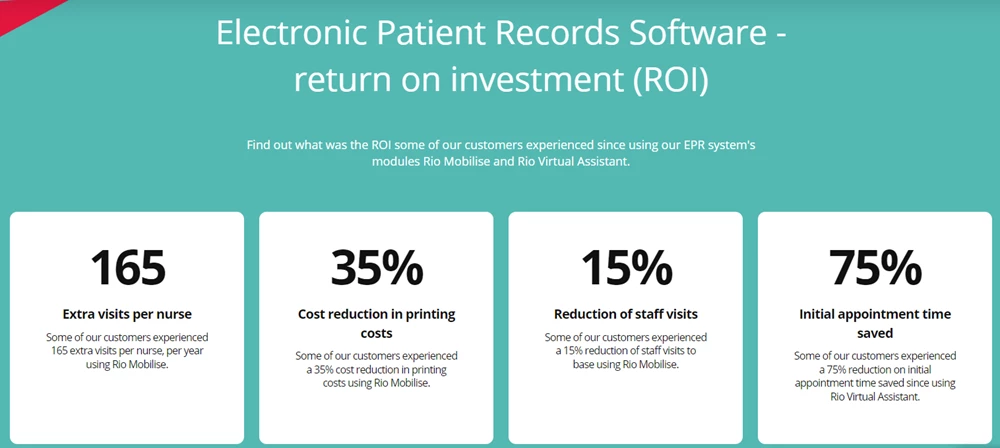
There are four areas where EHR systems can help healthcare organisations reduce cost:
- Staff workload (inc. stress and burnout)
- Data sharing
- Wider collaboration
- Accuracy of patient records
Staff Workload:
A large part of why healthcare organisations struggle is due to the work burden. Populations are growing, we’re still dealing with the backlog of care requests from the pandemic, and people are a lot more conscious about investigating ailments or concerns rather than waiting it out. This has resulted in more appointments than ever, but with tight budgets for public healthcare it has meant that waiting lists have grown exponentially. Organisations like the NHS are working flat out to make progress, but this has a toll on staff. Stress is a serious problem and after so long working under duress, it’s no surprise that there are people going sick – or even quitting their role – due to burnout.
This poses two financial problems: firstly, the person needs replacing. This is quickest done via agency staff, but these quick-fix hires are at a higher pay rate than salaried clinicians. The second problem is the expense of hiring new salaried staff, and then their training and development. An EHR system can alleviate the burden on these staff members by speeding up the data entry process for patient notes and automating other tasks, meaning more time can be focused on the patients themselves but also time can be clawed back to allow staff the proper respite to be fresh for the job.
Data Sharing:
Next, data sharing. The slow transfer of data between internal systems, teams and departments can hinder patient care and often misses ideal but small windows of opportunity to fit in appointments. With an EHR system integrated into a care organisation’s existing setup, patient records and medical data can be shared across a hospital or clinic setting in real-time. This means quicker processing of patient needs and appointment demands and a quicker invitation to an appointment – which can often catch or resolve an issue before it escalates. This is the cost saver – prevention.
Wider Collaboration:
Collaboration is a logical extension of this issue. Interoperability of software allows the integration to happen, but it also allows an organisation to collaborate with other providers as part of an Integrated Care System (ICS) or other regional partnership. With an EHR solution in place, there’s the potential for a healthcare organisation to save costs in areas of overlap between different providers and services.
Accuracy of records:
The final area we can reduce the electronic health record cost is by improving record accuracy. Paper-based records are okay but outdated and a risk issue. They also take up a lot of space and are costly to transport, and slow. Digital records are stored in a hard drive or in a cloud drive online and can be communicated instantly. This real-time access allows real-time updates, which means there can be one longitudinal record for all care providers to operate from – if an EHR solution is in place to provide that linkage. A central record means clinicians are operating from the same hymn sheet, and means they’re able to coordinate their knowledge and approach to both diagnosis and treatment. This means less waste via better prescriptions, and fewer mistakes that will waste medication or see a patient need additional services or perhaps even something serious enough to warrant a legal settlement. There are lots of areas of risk, and better clinical practices can avert them – but only with appropriate software in place to assist.
How much does EHR implementation cost?
The cost of implementing electronic health records is not a set scale. These costs vary per software provider, which means there’s no easy way to check via an electronic health record system cost calculator.
There are two costs to consider: the implementation (upfront cost) and the subscription (monthly or annual payments). These are affected by the term length of the contract between the vendor and the healthcare provider, as well as the number of registered users needing accounts for utilising the software.
At Access, we sell Rio Cloud and Rio EPR; two sides of the same coin that is electronic health records, but distinct programs in their own right that offer a more pre-configured EHR integration versus a more modular solution to handle an array of specialist care provisions. As well as contract length and users, the amount of modules you choose in our case will also impact the EHR implementation costs.
Software as a Service (SAAS) is the future though, and it’s an area that Access and Rio Cloud are growing into. Consumers want to keep costs low, and cloud-based applications – SAAS – are a way to avoid any onboarding costs. In the not-too-distant future it will be the default practice that EHR solutions are implemented this way, and those cost savings can only be a good thing for care provision.
EHR software prices
EHR software prices is our final point of order in this article. EHR pricing models differ from company to company as we’ve said, and the big complaint is that there are no EHR price comparison websites like with car insurance. Some do claim to offer such a function, but they are there to act as a middleman and want you to register with them and engage with them, when it’s far simpler to go direct to a software provider.
The important part for any prospective consumer is to make contact with organisations and to see what their solutions are like, through demos and discussion, and to assess costs. Typically, it is more cost-effective to be a bigger customer with more users. Economies of scale are involved and allow for a greater saving. A smaller care provider may find that the annual fees are acceptable but onboarding the software to be very expensive – which is prohibitive to providing good care and growing as a business.
As a rough estimate, you are looking in the low thousands of pounds or dollars to implement an EHR solution, though that figure will vary depending on the size of your organisation. For the subscription fees, these could range from thousands to hundreds of thousands – all depending on how many staff members are using the software. This is then further added to by the modules you choose. Some solution may be all-inclusive, but at Access - and other competitors - we offer the option to customise what functionality you need and will use. The more modules you choose, the greater the cost; both to implement the solution and to use it annually.

EHR costs – in conclusion
This brings us to the end of our article on the cost of electronic health records. We hope it has been insightful, but if you would like further information you can read about why EHRs are being pursued to keenly in our articles on the NHS Long Term Plan and our piece about the NHS Digital Capabilities Framework; guiding principles for digitisation in UK healthcare and how they aim to level-up care and deliver one, intelligent network.
Why not also speak to our Rio sales team for details about our EHR solutions, their functionality, and the costs involved should you partner with us. Research is everything when getting a good deal, so contact us today for a no-obligation chat about what Access has to offer you.